You may be already familiar with the controversy that a couple of newspaper articles have generated regarding the tweets of Lisa Adams, a woman who is terminally ill, and who has been openly blogging and tweeting about her journey as a patient diagnosed with an incurable cancer. She is not alone in doing this. Dr Kate Granger is also a young woman diagnosed with a terminal cancer, as well as a doctor. She too has chosen to share her experience online, including very personal feelings and pictures of her ordeal.
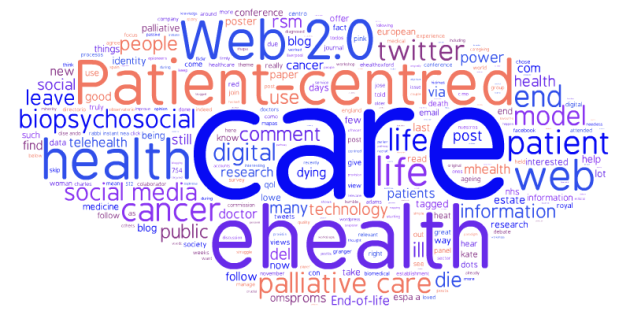
One could look at this anecdotes phenomenon from many angles, and indeed most have been covered: ethical, public health, medical, social media, patient engagement… To me, the essence of the debate is a very old one: it all boils down to a power struggle, because
the irruption of the Web 2.0 has fostered a paradigm shift within the healthcare landscape.
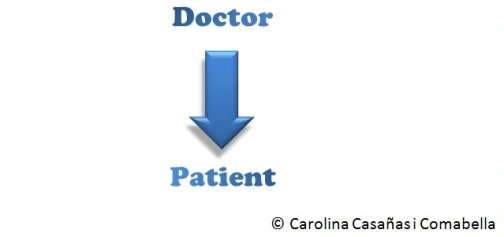
Not many years ago, the healthcare system was dominated by what has been called the biomedical model. In this model, doctors* knew best, and patients did not question what they were told. Patients were passive recipients of the medical knowledge. We could represent this model in a very simple diagram:
More recently though, things have changed. The biomedical model is slowly but steadily being replaced by the biopsychosocial model. There are many differences between this model and the traditional, biomedical model. I will only focus on the different doctor-patient interaction. In this model, patients take a proactive role. Instead of being passive, the patient has become an engaged and empowered stakeholder, thus changing the doctor-patient relationship:

In my opinion, the debate about patients’ tweets is a symptom that shows how the establishment struggles with this new paradigm. I think it’s interesting how so many people are scared of social media, because it gives power to the people. Until now, it was just us (doctors, journalists, politicians, scientists…) who told things the way we thought they were. Our vision of the world was the right one, and “the lay person” listened. But now, with the Web 2.0 (and this includes social media), everyone and anyone can tell things the way they think they are, and our version of the story is no longer the right one. And we are forced to listen.
It is time that the self-appointed experts give some room to the patients, because thanks in part to social media they are going to take the centre stage whether you like it or not. After all, is this not the essence of patient-centred care?
* Just to make this post easier to read, I chose to simplify and use the word “doctor”. Of course I mean the medical establishment, including nurses, psychologists, psychiatrists, physiotherapists and so on. I’m sure you understand what I mean when I say “doctor”.